As the COVID-19 outbreak response intensifies and the number of patients continues to grow, stakeholders are working hard to strengthen the health care community and ensure that sufficient capacity is available to meet the need. The President's unprecedented nation-wide national emergency declaration on March 13, 2020 notes that, "It is incumbent on hospitals and medical facilities throughout the country to assess their preparedness posture and be prepared to surge capacity and capability." This includes establishing additional intensive care unit (ICU) beds, procurement of additional personal protective equipment (PPE), and augmentation of professional staff.
As hospitals and other health care entities continue to navigate the COVID-19 response, below are ten tips to help ensure that they meet Federal Emergency Management Agency (FEMA) eligibility and compliance requirements for FEMA funding:
- Establishing Additional ICU Capacity. Some hospitals may be contacted by their respective Governor's Office or State Emergency Management Agency to get involved with the emergency response by increasing their ICU capacity, while others may be considering increasing their capacity to serve their respective communities. Building ICU capacity is expensive, but significant portions of these costs may be reimbursable by FEMA if done correctly. Hospitals should document any orders from public health officials and keep records of the need to support the increased capacity as necessary and reasonable.
- Federal Procurement and Contracting Considerations. Contracts must include all federal requirements, terms, and provisions. This can be done when signing, or existing contracts may be modified to ensure compliance. This is a fundamental eligibility requirement to receive FEMA reimbursement. FEMA's Procurement Disaster Assistance Team website has more details on the requirements. Also, make sure to document the procurement process and the emergency conditions requiring the expenditure. Although it may seem obvious and unnecessary right now, many of these costs will be reviewed and audited months or years later without the current pressures.
- Document Direction or Orders from Public Health Officials. Unlike typical FEMA declarations for storm damage, the pandemic nature of this disaster adds different requirements needed to substantiate costs. FEMA published guidance on March 19, 2020 indicating basic types of eligible emergency protective measures required by the COVID-19 response. In that guidance, FEMA stated, that "eligible emergency protective measures taken to respond to the COVID-19 emergency at the direction or guidance of public health officials may be reimbursed under Category B of FEMA's Public Assistance program." Thus, we recommend that before making significant expenditures with the expectation that FEMA will reimburse those costs, ensure the measures to be taken are at the written direction of a federal, state or local public health official and keep that written guidance with your procurement file. See more about this here.
- Confirm the "Applicant". Due to the unique considerations and each governor's preferences, ICU expansions may be done by either the hospital or directly by the state through an agreement with the hospital. Understanding upfront who will be responsible for applying for assistance to FEMA will drive contracting standards, responsibilities, and even funding. FEMA is attempting to create and implement a new expedited reimbursement system, but since it is a new process, FEMA is still weeks away from the Grants Portal being ready. Read more about that new process here.
- Understand and Discuss Payment of the Non-FEMA Cost-Share. Currently, even states that have been granted a Major Declaration are only eligible for reimbursement of a 75 percent federal share of eligible COVID-19 costs they incur. Twenty-five percent of millions or even billions of dollars is a significant amount. Although it is expected that this federal cost may be increased to 90 percent, at least for some states, hospitals should be aware and discuss with their state officials who will be responsible for the non-federal share.
- Track Volunteer and Donated Resources as Possible Credit for Non-Federal Share. When individuals and organizations donate resources to assist with response and recovery operations, the value of those donations may be used to offset the non-federal cost share. Hospitals should keep detailed logs of all volunteer hours and donations and even consider appointing a donation and volunteer coordinator to keep a centralized repository. Considering the amount of detail FEMA requires, these documents need to be kept as contemporaneously as possible. The below must be documented:
- The donated resource is from a third-party (a private entity or individual that is not a paid employee of the applicant or federal, state, territorial, or tribal government);
- The donated resource is necessary and reasonable for accomplishment of the project;
- The applicant uses the resource in the performance of eligible work and within the respective project's period of performance; and
- The applicant or volunteer organization tracks the resources and work performed, including description, specific locations, and hours.
- Align the Project's Scope with FEMA Guidance. Especially for significant construction costs related to ICU capacity, hospitals should carefully align their plans and scopes of work with the allowability for FEMA funding. The only category of Public Assistance work currently authorized is Category B Emergency Protective Measures, which must be "temporary" in nature. The March 19, 2020, FEMA Fact Sheet discusses the eligibility of emergency medical care including, "Temporary medical facilities and/or enhanced medical/hospital capacity (for treatment when existing facilities are reasonably forecasted to become overloaded in the near term and cannot accommodate the patient load or to quarantine potentially infected persons)." Thus, for construction of ICU facilities, hospitals must pay attention to the nuance between "enhancement" and permanent work. Hospitals should also document support that the work is needed because existing facilities are "reasonably forecasted to become overloaded".
- Consider Funding for Additional Staffing Costs. Generally, FEMA policy for reimbursement of staffing for emergency work by their employees follows this chart:
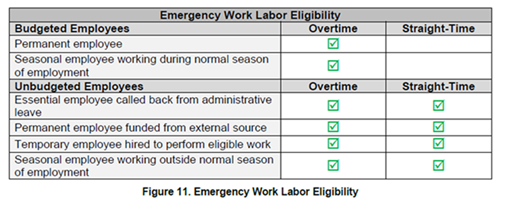
Hospitals contracting staff and/or temporarily hiring employees to perform COVID-19 treatment and support are eligible for both the worker's straight-time and overtime to be reimbursed. Costs of overtime of permanent employees may also be eligible if responding to the COVID-19 crisis. Hospitals should ensure their overtime policies are written, uniformly applied, and not contingent on federal funding.
- Document Escalation of Costs. We have seen reports across the country of supply and medical staff shortages causing higher than normal costs. When contracting, hospitals should attempt to get as many quotes as possible from contractors and suppliers and keep detailed documentation of those attempts, and also document the reasons of the escalating costs of these healthcare workers. FEMA requires that cost be "reasonable" in order to qualify for reimbursement. A cost is reasonable if in its nature or amount, it does not exceed that which would be incurred by a prudent person under the circumstances prevailing at the time the decision was made to incur the costs.
- Track All Funding - Finance Department Involvement is Critical. FEMA strictly prohibits duplication of benefits. Hospitals must be mindful and track all funding, including payments from patients, insurance, and state Medicare or Medicaid payments. All costs and funding sources must be closely tracked. If other funding is available for FEMA-eligible services or costs, including costs to construct additional capacity, FEMA may adjust otherwise eligible reimbursements. Of particular note, the third stimulus package, the CARES Act, passed on March 27 will provide considerable financial resources to health care entities for some costs. You can see our alert on that here.
Baker Donelson continues to monitor coronavirus developments and we will provide updates on funding opportunities as they become available. If you have any questions regarding this alert or the impact of the coronavirus (COVID-19) on your organization, please contact Danielle Aymond, Wendy Huff Ellard, Ernest B. Abbott, or any member of Baker Donelson's Disaster Recovery Team. Also, please visit the Coronavirus (COVID-19): What You Need to Know information page on our website.